What are Pressure Ulcers, Bedsores, and Pressure Wounds?
Pressure to the skin can interrupt blood flow, which over time causes skin to become starved of nutrients and oxygen. Skin that does not receive enough blood flow will begin to break down. Pressure injuries form either when the skin is under a lot of pressure for a short period of time, or when it is under a moderate amount of pressure for a long time.
These are known as bedsores, pressure ulcers (when open), pressure injuries, and decubitous ulcers (an outdated medical term still in use).
Bedsores are more likely to occur over areas of the body with less body fat or muscle between skin and bone, such as at the spine, tailbone, shoulder blades, hips, heels and elbows.
As we age, our skin becomes more delicate and vulnerable to wounds, tears, and abrasions. Nursing home caregivers are required to take precautions with residents’ skin. When nursing home caregivers are too busy, understaffed, or under-trained, skin wounds are going to become more common.
We investigate bedsore incidents in nursing homes on behalf of families to determine whether the wound was preventable, what efforts were taken to heal the wound or prevent development, and what efforts were taken to prevent infection.
What Nursing Home Standards Should Bedsore Lawyers Know?
Rules and regulations matter. Bedsore lawyers should know the federal nursing home regulations inside and out.
Federal regulations require nursing homes to prevent new wounds from forming unless they were clinically unavoidable because of the resident’s medical condition. Nursing homes are also required to prevent wounds from becoming infected.
In my experience litigating nursing home cases involving pressure ulcers, inadequate attention from nursing staff, inadequate training, and poor positioning all contribute to developing wounds.
One frequent cause of bedsores is when a resident is left in one position for an extended period of time, allowing pressure over a specific area of skin to damage the skin. Called a “deep tissue injury,” these types of wounds can develop from the inside out. These types of wounds can develop whether a resident is sitting or lying down.
Many nursing home residents who are unable to reposition themselves well will have a “turn and reposition q 2 hours” order, meaning a staff member should be helping the resident move to a new position at least every two hours. In an understaffed nursing home, that is an order that is much easier to check off in the books than actually get down with multiple residents.
Besides preventing the wounds from developing, nursing staff have to timely change dressings on existing wounds, and do so in a sanitary way to prevent infection. Healthcare-acquired infections are a serious risk in nursing homes. Bedsores that are not treated consistently will worsen, and can lead to infection, sepsis, or death.
Incontinent nursing home residents are especially at risk and should be more closely monitored. Being left in soiled clothing cause open wounds which may develop into bed sores, or lead to infection.
Nursing homes must ensure that residents are well monitored, bed- or wheelchair-bound residents are frequently repositioned, pressure-reducing tools like special mattresses, pillows, and pads are used, incontinent residents are kept clean and dry, and wound dressings (bandages) are regularly changed in a sterile way.
All of that can take a lot of staff time and attention. When a nursing home puts its own profits over resident safety, there may not be adequate staff to take that level of care.
Read Nursing Home Bedsore Lawyer William Eadie’s Article on How Recent Changes to Nursing Home Regulations Affect Nursing Home Abuse Cases
Do Bedsores Mean the Nursing Home was Negligent?
Bedsores might be a sign of neglect, and neglect can affect residents in other ways, too—dehydration, malnutrition, falls from lack of monitoring, even infections caused by inadequate dressing changes or unsanitary conditions.
When a nursing home neglects obvious conditions, it can rise to the level of abuse.
Nursing home neglect contributing to bed sores can include:
- Bedbound or wheelchair bound (immobile) residents to remain in the same position for too long
- Failing to provide proper nutrition or fluids, which can make residents extremely vulnerable to skin breakdown, infections, sepsis, and death
- Allowing residents to have moist skin for too long, from not changing soiled adult diapers or wet bed sheets.
- Failing to check residents regularly skin problems
- Failing to notify the family and physician upon development of sores so that proper treatment may be rendered
Nursing homes are also required by federal and Ohio regulations and laws to notify designated representatives—and doctors—of significant changes in condition. Nursing home bedsore lawyers should know these regulations inside and out. This is not just another “personal injury” case.
In some cases, a nursing home may not notify the family or physician of the existence of bedsores.
Failure to report the existence of bedsores will result in the resident being left with untreated open wounds. Unrecognized pressure sores or inappropriately treated ulcers could result in sepsis, shock, gangrene, or death.
Finding the Best Nursing Home Bedsore Lawyer for Your Case
Any attorney who handles “personal injury” cases will want your bedsore lawsuit, because they seem easy: an open wound, someone died or became seriously injured.
But most “personal injury” attorneys don’t regularly handle nursing home cases. They have no idea how to properly investigate the larger issues involved, understaffing, systemic failures, even identifying the full impact of a wound on a person’s health. And they may not be used to understanding and communicating the loss of an older person on a family.
We’ve handled cases where other lawyers do not even recognize that a nursing home injury led to the resident’s death weeks later.
There’s no excuse for trusting a nursing home case to a lawyer who does not focus on nursing home cases. That’s why many of our cases come from other lawyers who recognize our experience and success–even from personal injury lawyers!
To find the best bedsore lawyer for your case, start by finding lawyers who focus on nursing home cases. They shouldn’t be doing lots of other things, too. You want lawyers who have not just settled, but taken nursing home cases to trial. Ask them about that!
If you would like to discuss your loved one’s situation, injuries, or death at a nursing home, call us at 216-777-8856. While we handle cases throughout Ohio, we’re happy to consult on extreme cases nationwide. If you are outside Ohio, we can help you find qualified counsel in your state.
Filing a Bedsore Lawsuit in Ohio
Bedsore lawsuits require a deep knowledge of the laws and regulations governing nursing homes–they are not just another personal injury case.
Under Ohio law, nursing homes can be held liable for allowing preventable bedsores from developing. We limit our practice to the most extreme cases, because we attack every case as if we’re going to go to trial.
If you’re reading this and the situation is ongoing, there are steps you can take to help us best represent your family.
Consider taking pictures of any wounds, noting the time and date. Photos can be some of the most important evidence in a case involving bedsores.
Also, keep notes about your conversations and observations. It can be important to know the names of staff providing care—which the nursing home must provide under Ohio law upon request—especially since there can be high turnover at these facilities. The person may not even work there by the time you call us.
Nursing home cases are generally considered “medical claims” in Ohio, which means you may have as little as 1 year form the date of negligence in which to sue. This is called the “statute of limitations.”
There are ways to extend that time, and plenty of complicated factors to consider as to when the clock starts running. Get a nursing home lawyer on the investigation as early in the process as you can.
I hate to get calls from families after the time has run. It isn’t their fault–they were worried about things like helping the person recover, funerals, mourning–but the law still takes their right to sue away.
We also investigate the corporate structure of nursing homes to find out who the real decision makers are. Often there are 3 or more companies involved beyond that individual facility controlling the money and staffing levels. Bedsore lawyers should get to them, too, in their investigation.
Are pressure wounds preventable?
Preventing bedsores is the best options–and nursing homes know it’s their job to prevent avoidable bedsores.
Bedsores are preventable if nursing homes take appropriate care. Unless a resident is terribly ill—such as kidney or other organ failure—suffering from vascular / circulatory issues, or otherwise severely compromised, appropriate care should prevent bedsores from developing.
If a loved one develops bedsores that worsen or become infected, it may be a sign of neglect, malnutrition, dehydration, or all three. Ohio and federal nursing home regulations dictate the level of care required, and sometimes a nursing home’s own policies add to that level of care. When we investigate nursing home cases involving bedsores, we answer the question whether they were preventable, and whether the nursing home violated its obligations in allowing them to form.
When nursing homes fail to provide this level of care to prevent, help heal, and avoid infection of pressure wounds, it may be liable for any resulting damages.
We have investigated and tried cases involving nursing home negligence allowing pressure wounds to develop and even become infected. Please contact us to discuss your potential case. You’ll get our candid evaluation at no cost.
Nursing home caregivers should be well-versed in the techniques necessary to prevent bedsores, including:
- Daily skin checks
- Repositioning
- “Off-loading” pressure points
- Positioning residents at a 30 degree angle to reduce pressure
- Properly employing pressure-relieving devices like foam padding, air mattresses, and pillows
- Keeping residents, clothing, and bedding clean and dry
- Frequent, multiple daily checks
Nursing homes can be liable for bedsores caused by failing to adequately monitor, assist, or reposition residents having limited mobility.
Pressure Wound Complications from Bad Care
Unraveling the cause of someone’s death in a nursing home can be complicated. Serious wounds can lead to complications that cause death, but it may not be obvious.
If a wound is allowed to develop to Stage III or IV, serious and life-threatening complications can develop. Bedsore lawyers should know these complications, so they can identify cases where a bedsore caused more problems.
These include:
- Sepsis: the presence in tissues of harmful bacteria and their toxins, typically through infection of a wound. This can lead to organ damage or failure, which can lead to septic shock, respiratory failure, and death. This is a medical emergency.
- Cellulitis: a potentially serious bacterial skin infection that may appear as a swollen, red area of skin that feels hot and tender. Without treatment, the infection may spread to the blood (sepsis), bones (osteomyelitis), joints (septic arthritis), or to the brain and spinal cord membranes (meningitis).
- Gangrene: localized death and decomposition of body tissue, resulting from either obstructed circulation or bacterial infection, a medical emergency that requires immediate removal of the infected area by debridement or amputation.
- Osteomyelitis: inflammation of bone or bone marrow, usually due to infection, which can spread from surrounding tissue or blood, and requires treatment with antibiotics and possibly surgical removal.
- Septic arthritis: is a painful infection in a joint that can occur when a penetrating injury delivers germs directly into the joint. Requires treatment with antibiotics or surgery to remove infected areas.
- Necrotizing fasciitis: a flesh-eating bacteria that causes rapid tissue death (necrosis) requiring immediate medical intervention including antibiotics and removal of dead tissue.
If your loved one was in a nursing home and suffered from one of these complications from a wound, call us at 216-777-8856.
Are the Nurses and Aides to Blame for Bedsores?
Nursing staff is often understaffed and over worked by greedy nursing home corporations.
In a very obvious way, yes, nurses and aides–the people responsible for evaluating skin, providing the positioning and offloading to prevent or help heal bedsores, and the rest–are “responsible” for bedsores.
But it is important to realize that in the nursing home bedsore cases we’ve handled, the nurses and nursing aides are really victims, too. What I mean by that is that the nursing home company under-staff the facility, meaning the nurses have to try and do too much in too little time.
The result is people not getting care. And one of the easiest things to skip are detailed skin checks, re-positioning residents, and changing undergarments.
The natural result is skin breakdown and infections.
Is it really the nursing staff’s “fault” that they can’t do the impossible? Of course not.
Now, you may be angry at them, or specific staff. We get that. They seem rude, short tempered, lazy, disinterested, you name it. But in a very real sense, they’re trying to cope with a terrible situation: their company is putting its own profit over resident care.
That’s why we don’t sue the nurses directly, or beat them up at trial. We get under the surface to the real, root cause of the bedsore. That’s what bedsore lawyers should do.
Otherwise, this seems like just one mistake, or failure, by a few nurses. When the real problem is a system set up by the nursing home company that was going to lead to injury or death no matter what.
Common Pressure Sore Locations
Where pressure ulcers are likely to develop depends on where the person spends time under pressure. (Image courtesy of the JAMA Network, by Cassio Lynm, MA, available here)
Pressure sore lawyers should be aware of the common locations for bedsores, so they can compare that with the person’s condition. And to understand when unusual bedsores show up so they can investigate why.
For people who use a wheelchair, pressure sores often occur on skin over the following sites:
- Tailbone or buttocks
- Shoulder blades and spine
- Backs of arms and legs where they rest against the chair
For people who are confined to a bed, common sites include the following:
- Back or sides of the head
- Rim of the ears
- Shoulders or shoulder blades
- Hip, lower back or tailbone
- Heels, ankles and skin behind the knees
Risk Factors for Bedsores
Nursing home staff–and bedsore lawyers–must be aware of the risk factors for skin breakdowns and wounds, which include:
- Age: the older we are, the more delicate and vulnerable our skin becomes. Older people have less efficient circulation, less elastic skin, and fewer protective fat stores under the skin, which provides padding.
- Poor nutrition. Older people are at a higher risk of poor nutrition and dehydration, which can compound other risk factors such as aging skin tissue and problems with mobility. Residents who cannot feed themselves in particular are more vulnerable to nutrition issues, that can lead to skin breakdowns.
- Dehydration, which can set in quickly, can lead to rapid health decline, including skin breakdowns.
- Underweight residents;
- Limited mobility, especially bedbound or wheelchair bound.
- Incontinent residents, which leads to damp skin, and possibly less sanitary conditions.
- Friction caused by turns, lifting, or pushing a resident too rapidly;
- Shear resulting from a resident sliding down in a bed or chair or from being positioned incorrectly; and
- Serious medical conditions affecting the skin, circulation, or immune system, including diabetes, kidney disease, chronic obstructive pulmonary disease (COPD), which can lead to too little oxygen in the blood, heart failure, and peripheral artery disease.
People who have difficulty with mobility are always more likely to develop pressure ulcers, especially with inadequate care.
Bedsore Staging
Bedsores or pressure wounds fall into four stages, as well as “suspected deep tissue injuries” and “unstageable.” When nursing homes do a bad job staging a bedsore over time, that can be a violation of government nursing home regulations.
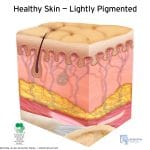
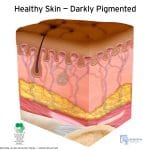
Healthy Skin
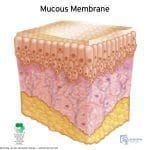
Understanding how to stage pressure ulcers requires understanding what healthy skin is, and how it can differ when looking for signs of sores based on skin pigmentation and whether it is really skin or mucous membranes.
- Staging a nursing home pressure ulcer starts with knowing what healthy skin is. This is a cross section image of lightly-pigmented healthy skin. Pigmentation can make staging pressure ulcers (commonly called bedsores) more difficult. (Courtesy of the National Pressure Ulcer Advisory Panel.)
- This is a cross section image of darkly-pigmented healthy skin. Pigmentation can make staging pressure ulcers (aka “bedsores”) more difficult. (Image courtesy of the National Pressure Ulcer Advisory Panel)
- The moist lining of body cavities like the mouth and nose–called the mucous membrane–can be next to normal skin areas that have pressure ulcers, but you cannot use the same assessments to determine pressure ulcers. For example, these areas do not blanch like normal skin. (Image courtesy of the National Pressure Ulcer Advisory Panel)
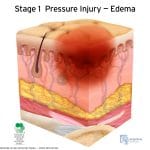
Stage I
At the beginning of a pressure sore—Stage I—you will see:
- Unbroken skin
- The skin appears does not blanch—lighten when pressed briefly—and looks red on people with lighter skin color, or discolored on people with darker skin tones.
- The skin may be tender, firm, soft, warm or cool compared with the normal, surrounding skin.
Here are images of stage 1 sores:
- This is a cross section image of darkly-pigmented skin with a Stage 1 pressure ulcer (also called a bedsore, decubitous ulcer, or pressure wound). Pigmentation can make staging pressure ulcers more difficult because you cannot see discoloration or blanching as easily. (Image courtesy of the National Pressure Ulcer Advisory Panel)
- Cross section of lightly-pigmented skin with a stage 1 pressure ulcer or bedsore, represented as a red area extending below the skin’s surface. Red areas are easier to observe on lighter skin. (Image courtesy of the National Pressure Ulcer Advisory Panel)
Here is some information on blanching and edema:
- When a patient’s skin loses redness with pressure it is called “blanchable”; “unblanchable” skin does not. A stage 1 bedsore is defined as non-blanchable. (Image courtesy of the National Pressure Ulcer Advisory Panel)
- This is a cross section image of skin with a Stage 1 pressure ulcer (also called a bedsore, decubitous ulcer, or pressure wound), with excess fluid collecting in the skin, called “edema.” Edema increases the risk of developing a skin ulcer, and can complicate healing, by compressing small blood vessels. (Image courtesy of the National Pressure Ulcer Advisory Panel)
Stage II
At stage II, a pressure ulcer is more apparent as a wound:
- The outer layer of skin is damaged or lost, and the under layer is damaged.
- The wound may be shallow and pinkish or red.
- The wound may look like a fluid-filled blister or a ruptured blister.
- It is possible for skin at this stage to be damaged beyond repair or die.
A stage 2 bedsore, which presents as partial thickness loss of dermis and a shallow open wound with a red or pink wound bed, or as an intact or open/ruptured serum-filled blister. (Image courtesy of the National Pressure Ulcer Advisory Panel)
Stage III
At stage III, the pressure ulcer has become a deep wound:
- The wound gets below the skin to the level of fat below
- The wound appears “crater” like
- There may be dead (necrotic) tissue on the bottom of the wound
- The damage may extend or tunnel beyond the primary wound below layers of healthy skin.
- Stage 3 pressure wound showing wound open to fatty layer (full-thickness tissue loss), but not to bone or muscle (which would be stage 4). Devascularized yellow tissue (“slough”) may be present but does not hide the bottom of the wound. (Image courtesy of the National Pressure Ulcer Advisory Panel)
- A Stage 3 pressure wound (bedsore or pressure ulcer) with rolled or curled-under closed wound edges, called “epibole.” Epibole is usually lighter colored than surrounding skin, with a raised and rounded appearance. (Image courtesy of the National Pressure Ulcer Advisory Panel)
Stage IV
A stage IV ulcer shows large-scale loss of tissue:
- Muscle, bone or tendons may be visible.
- There is likely dead tissue—yellow or black—at the wound bottom.
- The damage often tunnels or extends below layers of healthy skin around the wound.
Stage 4 pressure wound showing wound open to bone, tendon, or muscle. Devascularized or dead tissue (slough or eschar) may be present, but the bottom of the wound can be seen. (Image courtesy of the National Pressure Ulcer Advisory Panel)
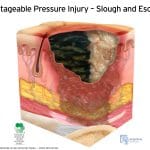
Unstageable
It can become impossible to see how deep a wound is when its surface is covered with yellow, brown, black or dead tissue. At that point, the wound is considered unstageable.
- Staging a nursing home pressure ulcer becomes impossible when the open wound is filled with devitalized yellow tissue (“slough”) or black, dead skin (“eschar”). This is called “unstageable.” It’s important to note that eschar is not a scab. (Courtesy of the National Pressure Ulcer Advisory Panel.)
- An unstageable open pressure wound with dark dead skin (eschar) hiding the depth of the wound. (Image courtesy of the National Pressure Ulcer Advisory Panel)
Deep tissue injury
A deep tissue injury is characterized as:
- Unbroken, discolored skin (purple or maroon)
- A blood-filled blister is present.
- The area is painful, firm or mushy.
- Compared with the healthy surrounding skin, the injured area will be warmer or cooler temperature
- In people with darker skin, a shiny patch or a change in skin tone may develop.
Deep tissue injury is a term proposed by the National Pressure Ulcer Advisory Panel to describe pressure ulcers that do not fit within the standard staging, perhaps presenting as unbroken skin but being much more serious than a Stage I bedsore. (Image courtesy of the National Pressure Ulcer Advisory Panel)
Treating Pressure Ulcers
The most important part of treating pressure ulcers—besides preventing them—is to recognize them quickly and provide consistent care to keep them from becoming worse. We’ve seen too many cases where a nursing home drops the ball in follow-up care, meaning wounds get worse, or even infected.
Care starts with alleviating the underlying cause, using creams or gels, and pressure-relieving devices to prevent additional sores. More serious wounds require wound dressings / bandages, advanced wound care, special padding or mattresses, or surgery.
Special wound doctors can remove dead / necrotic tissue at the bedside, called “debriding” a wound.
Protecting Elderly Skin
(Re)Positioning
Frequent position changes relieve pressure and allow for better blood flow to skin. Repositioning is an important way to prevent pressure ulcers and encourage healing of existing ulcers. At-risk residents should be provided a repositioning schedule such as being turned or moved every couple hours, or even 15 minutes for people at significant risk.
Repositioning should consider:
- ability of the person to independently reposition
- educating any staff or caregivers about proper repositioning
- sitting position and posture
- lying position
- supporting feet, arms, neck, trunk, and head
- using any necessary equipment and supports
Pressure Relieving Devices like Cushions
Air mattresses, cushions, and other pressure-relieving devices can help reduce pressure points.
Nutrition
Dietitians understand residents at risk of pressure ulcers, or healing open wounds, need more nutrition—especially protein—to keep their skin healthy or repair wounds. Adequate nutrition is a critical part of preventing and healing pressure sores. Residents at-risk for wounds should be seen by a registered dietician in order to develop an appropriately balanced diet to promote healing.
Dressings and Topical Treatments
Wounds can be protected by barrier creams, gels, and ointments, which can help to protect the wound from infection and promote healing.
There are wound treatments, including dressings, designed specifically to help heal, or stop progression, or pressure wounds. Special wound dressings can reduce pressure and support healing.
Hydrocolloid dressings are a specialized dressing for wounds that provide unique benefits. As described by Advanced Tissue, “Hydrocolloid dressings have an active surface treated with a gel-forming substance consisting of pectin, carboxy-methylcellulose, polymers and other adhesives. They are an opaque, flexible, wafer that adheres to the skin. When in contact with wound exudate, the polymers absorb the fluid and swell, forming a gel which is confined within the structure of the material.” They work best with wounds that are not infected. They provide some benefits, including:
- Minimal Disruption to Healing—needing application every 3-7 days, there is less disruption of healing, room for infection through changing dressings, and less intensive staff needs (meaning less risk of staff missing dressing changes).
- Impermeable to Bacteria
- Adheres Only to Intact Skin
- Easy to Apply
Alginate dressings contain substances like calcium and sodium that help the wound to heal faster, and are made of natural materials.
Antibiotics
Whether topical, oral, or IV, antibiotics are critical for stopping infections before they develop to systemic infections or sepsis. Infections place an additional strain, beyond healing the wound, on a person’s body energy.
Surgical Debridement
Cutting away dead or necrotic skin is called “debridement.” Besides using scalpels, wound specialists can also use: (1) cleansing irrigation, washing away dead tissue with high-pressure jets of water; (2) removing dead tissue with sound waves, called “ultrasound”; and (3) laser tissue removal treatment.
Debridement can be extremely painful. Local anesthetics can be employed to help reduce pain.
Surgery
When a pressure ulcer gets severe—State III or IV—surgery may be needed to close the wound. But the resident needs to be healthy enough to undergo such surgery, and resist infection.
Vacuum Treatments
Wound vacuums, called “wound vacs,” or negative-pressure therapy, use vacuum pressure on the wound to help close, extract moisture, and reduce infection risk.
Maggot Therapy
Although it might seem distasteful, “biological debridement” or maggot therapy uses larvae to remove dead tissue while leaving healthy tissue unharmed. Maggots also release bacteria-killing chemicals, which can make infection less likely. This is considered a safe and effective debridement treatment.

 100% Secure and Confidential
100% Secure and Confidential